The link between the Brain-gut axis and mental health has gained significant attention in recent years as scientists uncover the intricate connection between brain and gut. Often referred to as the “brain-gut axis,” this bidirectional communication network highlights how the gut and brain interact in ways that influence our emotions, cognition, and overall mental health. In this comprehensive article, we will explore how gut health impacts mental well-being, the role of the microbiome in this process, and how improving gut health can lead to better mental health outcomes. As of late 2025, groundbreaking research continues to reveal the profound implications of this axis for conditions like anxiety, depression, and even neurodegenerative diseases.
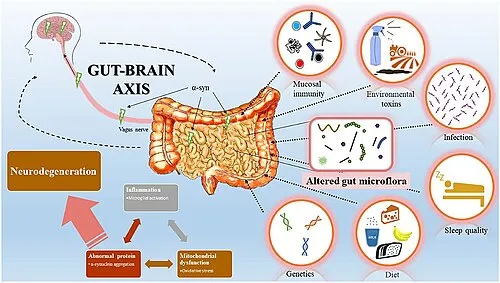
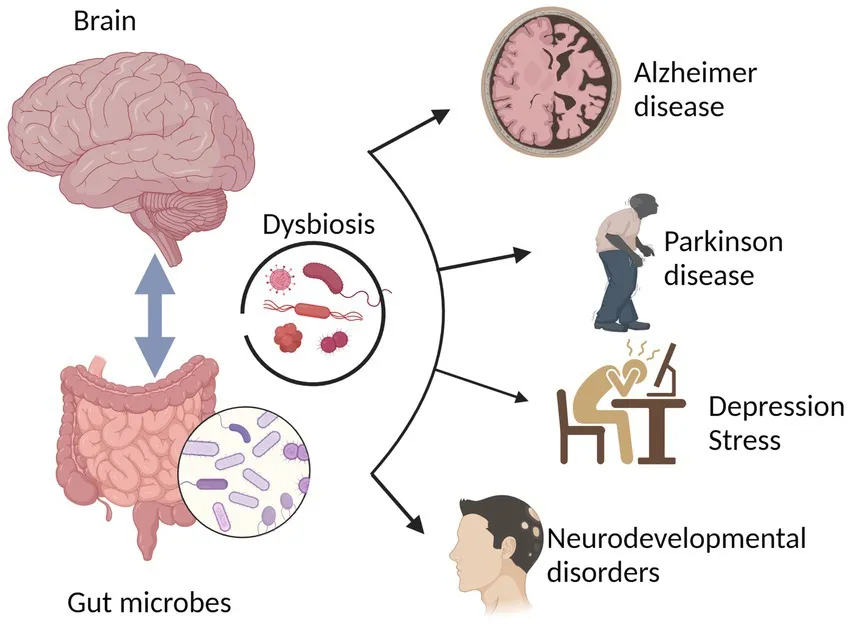
Recent studies from 2025 emphasize the bidirectional nature of the brain-gut axis, where gut dysbiosis can trigger neuroinflammation, contributing to mood disorders, while stress from the brain alters gut permeability and microbiota composition. This evolving understanding positions the gut microbiome as a potential therapeutic target for mental health interventions.
Understanding the Brain-Gut Axis
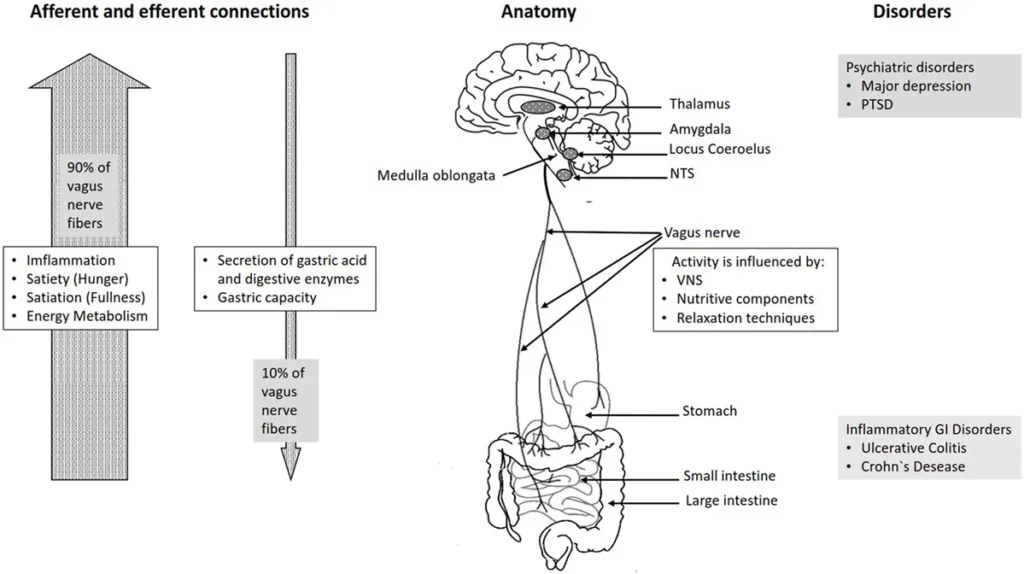
The brain-gut axis refers to the complex communication network between the central nervous system (CNS) and the enteric nervous system (ENS), which governs the gastrointestinal tract. This network allows the gut and the brain to send signals to each other through various pathways, including the vagus nerve, hormones, and immune system signals.
Key Components of the Brain-Gut Axis
- The Central Nervous System (CNS): The CNS includes the brain and spinal cord, playing a vital role in processing and regulating emotions, thoughts, and behaviors. It receives inputs from the gut that can modulate mood and cognitive function.
- The Enteric Nervous System (ENS): Often called the “second brain,” the ENS consists of a network of neurons lining the gut. It controls digestion and plays a role in gut-brain communication, independently managing gastrointestinal functions while relaying information to the CNS.
- The Vagus Nerve: This cranial nerve connects the brain to various organs, including the gut. It is a key player in transmitting signals between the gut and brain, influencing heart rate, digestion, and emotional responses.
- Gut Microbiome: The gut microbiome consists of trillions of microorganisms, including bacteria, viruses, and fungi, that inhabit the digestive system. It has a profound impact on gut health and overall well-being, producing metabolites that signal the brain via neural, endocrine, and immune pathways.
In 2025, advanced organ-on-chip technologies and multi-omics analyses have deepened our insights into these components. For instance, research highlights how the vagus nerve mediates anti-inflammatory effects, potentially alleviating symptoms in conditions like long COVID and Parkinson’s disease. Dysregulation in this axis is linked to increased intestinal permeability, allowing inflammatory molecules to affect brain function.
The axis’s bidirectional nature means psychological stress can alter gut microbiota, while microbial imbalances can exacerbate stress responses via the hypothalamic-pituitary-adrenal (HPA) axis. This interplay underscores why gut health is pivotal for mental resilience.
How Gut Health Affects Mental Well-being
The gut microbiome has a significant influence on mental health through several mechanisms. Imbalances in gut bacteria, known as dysbiosis, can disrupt this communication network and contribute to mental health issues, such as anxiety, depression, and stress.
The Role of the Gut Microbiome
The gut microbiome plays a crucial role in maintaining mental health by regulating the production of neurotransmitters, hormones, and immune responses. Research has shown that a healthy gut microbiome can positively impact mood and cognitive function, while an unhealthy microbiome can contribute to various mental health disorders.
- Neurotransmitter Production: The gut is responsible for producing key neurotransmitters, including serotonin, dopamine, and gamma-aminobutyric acid (GABA). Serotonin, often called the “feel-good” neurotransmitter, is primarily produced in the gut. Low levels of serotonin have been linked to mood disorders such as depression and anxiety. Gut bacteria influence tryptophan metabolism, the precursor to serotonin.
- Immune System Regulation: The gut houses a significant portion of the body’s immune cells. An imbalance in the gut microbiome can lead to inflammation, which is associated with mental health disorders. Chronic inflammation has been linked to depression, anxiety, and cognitive decline.
- Gut-Inflammation Link: Inflammatory molecules produced in the gut can travel through the bloodstream and cross the blood-brain barrier, influencing brain function. This can lead to brain inflammation, which has been associated with mood disorders and impaired cognitive abilities.
Recent 2025 studies reveal distinct microbial signatures in resilient individuals, with higher levels of bacteria promoting anti-inflammatory metabolites. Dysbiosis is implicated in neuropsychiatric conditions, including PTSD and bipolar disorder, where reduced diversity correlates with symptom severity.
Short-chain fatty acids (SCFAs) from microbial fermentation act as key mediators, modulating neuroinflammation and HPA axis activity. Interventions targeting these pathways show promise in restoring balance.
Gut-Brain Communication and Mental Health Disorders
Impaired communication between the gut and brain is believed to contribute to the development of several mental health disorders, including:
- Anxiety: Anxiety disorders are often linked to dysbiosis, where harmful gut bacteria outweigh beneficial ones. An imbalanced gut microbiome can trigger anxiety symptoms by altering the production of neurotransmitters and increasing inflammation. Studies in 2025 link low SCFA-producing bacteria to heightened anxiety.
- Depression: Low levels of beneficial gut bacteria have been associated with depressive symptoms. Dysbiosis can reduce serotonin production, leading to mood disorders and diminished emotional well-being. Meta-analyses confirm heterogeneous but promising reductions in depressive symptoms via microbiome modulation.
- Stress: Chronic stress affects gut health by altering the composition of gut bacteria and increasing gut permeability. In turn, gut dysbiosis can exacerbate stress by impairing gut-brain communication, creating a vicious cycle of stress and poor gut health.
Emerging research extends this to neurodegenerative diseases like Parkinson’s, where gut-originating inflammation may precede brain pathology. Long COVID cognitive symptoms also involve vagus nerve disruptions from gut dysbiosis.
How to Improve Gut Health for Better Mental Well-being
Improving gut health can have profound effects on mental well-being. Here are some evidence-based ways to promote a healthy gut, which can help support brain function and improve emotional health.
Dietary Changes
A well-balanced diet is essential for maintaining a healthy gut microbiome. Nutrient-rich foods can promote the growth of beneficial bacteria while minimizing harmful ones.
- Probiotics: Probiotics are live bacteria that support gut health. They can be found in fermented foods such as yogurt, kefir, sauerkraut, and kimchi. Consuming these foods can increase the number of beneficial bacteria in the gut and improve gut-brain communication.

- Prebiotics: Prebiotics are fibers that feed beneficial gut bacteria. Foods like garlic, onions, asparagus, and bananas are rich in prebiotics and help maintain a healthy gut microbiome.
- Fiber-Rich Foods: A diet high in fiber supports healthy digestion and promotes the growth of beneficial gut bacteria. Whole grains, fruits, vegetables, and legumes are excellent sources of fiber.
- Omega-3 Fatty Acids: Found in fatty fish, flaxseeds, and walnuts, omega-3 fatty acids have anti-inflammatory properties that can support both gut and brain health.
The Mediterranean diet, rich in these elements, consistently shows benefits for mood and microbiome diversity.
Lifestyle Changes
In addition to diet, certain lifestyle changes can promote gut health and enhance mental well-being.
- Stress Reduction: Chronic stress negatively impacts gut health. Incorporating stress-reducing techniques, such as mindfulness meditation, deep breathing exercises, or yoga, can support both mental and gut health.

- Regular Physical Activity: Exercise has been shown to positively impact the gut microbiome by increasing the diversity of beneficial bacteria. Regular physical activity can also reduce inflammation and improve mood by stimulating the production of endorphins.
- Sleep Hygiene: Adequate sleep is crucial for maintaining both gut and brain health. Poor sleep quality can disrupt the gut microbiome and impair cognitive function, leading to mood disorders.
- Avoid Excessive Antibiotic Use: Antibiotics can disrupt the balance of gut bacteria by killing both harmful and beneficial microorganisms. Use antibiotics only when necessary and consult a healthcare professional about probiotic supplementation during antibiotic treatment.
Probiotic and Prebiotic Supplements
For those who cannot consistently incorporate probiotic and prebiotic-rich foods into their diet, supplements are available. However, it is important to consult a healthcare professional before starting any new supplement regimen. Psychobiotics—specific strains like Bifidobacterium longum and Lactobacillus helveticus—show targeted benefits for anxiety and depression in 2025 trials.
Key Steps for Improving Gut Health
- Consume Probiotic and Prebiotic Foods: Incorporate fermented foods and high-fiber foods to nourish your gut.
- Reduce Stress: Practice stress management techniques to promote a healthy gut-brain connection.
- Exercise Regularly: Engage in physical activity to support gut health and improve mood.
- Get Adequate Sleep: Maintain a consistent sleep routine to enhance gut function and mental well-being.
- Limit Antibiotic Use: Use antibiotics cautiously to avoid disrupting the balance of gut bacteria.
Combining these with emerging therapies like fecal microbiota transplantation or precision psychobiotics offers personalized approaches.
Conclusion
The brain-gut connection underscores the importance of maintaining a healthy gut for optimal mental well-being. The gut microbiome, neurotransmitter production, and immune system regulation all play pivotal roles in this relationship. By adopting a healthy lifestyle, including a nutrient-rich diet, regular physical activity, and stress management techniques, you can improve gut health and support your mental well-being. As research into the brain-gut axis continues into 2025 and beyond, the importance of gut health in managing mental health will only become more evident, paving the way for innovative, microbiome-targeted therapies.
For more
For more exclusive influencer stories, visit influencergonewild






