
The Realities of Delayed Diagnosis: Causes, Consequences, and What You Can Do About It
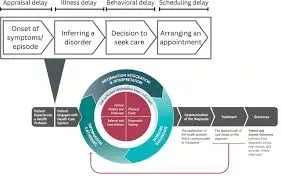
Early diagnosis has long been recognised as one of the most critical factors in achieving positive health outcomes. When medical conditions are identified at an early stage, patients often benefit from more effective treatment options, faster recovery, and a significantly improved quality of life. However, in the UK, increasing pressure on the healthcare system has made timely diagnosis increasingly difficult. NHS waiting lists, combined with lingering pandemic backlogs, have placed referral and diagnostic pathways under unprecedented strain.
For millions of patients, this reality means prolonged uncertainty, worsening symptoms, and missed treatment opportunities. Delays that occur quietly—before a specialist appointment or diagnostic test even takes place—are particularly concerning, as they often go unnoticed until serious harm has already occurred. These “invisible” delays not only threaten physical health but also carry profound psychological consequences.
This article explores the scale of delayed diagnosis in the UK, the conditions most affected, the mental and physical toll on patients, how individuals can navigate the healthcare system when something feels wrong, and when legal support may be appropriate following a delayed diagnosis.
The Scale of NHS Waiting Lists and Diagnostic Delays
The pressure on NHS England’s waiting lists has reached historic levels. As of August 2025, approximately 6.23 million people were waiting for treatment within NHS England. Alarmingly, nearly three million of those individuals had not received any specialist appointment or diagnostic test since being referred by their GP.
Even more concerning is that over one-third of these patients had already exceeded the NHS’s 18-week standard for referral-to-treatment. This benchmark exists to protect patients from prolonged delays, yet for many, it has become an increasingly unrealistic target rather than a guaranteed standard of care.
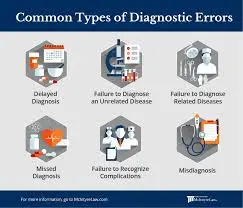
Invisible Delays and Their Hidden Risks
While long waits for surgery or treatment often receive public attention, delays earlier in the pathway—such as referral processing, initial specialist appointments, and diagnostic testing—can be far more dangerous. These early-stage delays are frequently invisible, leaving patients unaware that critical time is being lost.
Invisible delays can result in:
- Missed treatment windows
- Disease progression before diagnosis
- Reduced effectiveness of treatment options
- Increased patient anxiety and emotional distress
For conditions where early intervention is crucial, even small delays can significantly alter outcomes.
Common Conditions That Suffer from Delayed Diagnosis
A rapid evidence assessment shows that delayed diagnosis disproportionately affects chronic and serious conditions where symptoms may be vague, slow-developing, or easily mistaken for less serious issues. Limited consultation time and systemic pressures further compound the problem.
Chronic Conditions with High Rates of Undetected Cases
Chronic Obstructive Pulmonary Disease (COPD)
COPD often develops gradually, with early symptoms such as breathlessness or coughing being dismissed as ageing, smoking-related issues, or minor respiratory infections. Delayed diagnosis prevents early intervention that could slow disease progression and improve long-term lung function.
Dementia
Dementia remains significantly underdiagnosed, particularly in its early stages. Memory changes, confusion, and personality shifts are often attributed to stress or normal ageing, delaying assessment and access to support services that can improve quality of life.
HIV
Despite advances in testing and treatment, HIV still has a substantial number of undetected cases. Non-specific early symptoms and social stigma can discourage testing, leading to delayed diagnosis and increased risk of transmission and long-term complications.
Type 1 Diabetes
Type 1 diabetes can develop rapidly, yet its early symptoms—fatigue, weight loss, increased thirst—are often misinterpreted. Delayed diagnosis increases the risk of diabetic ketoacidosis, a life-threatening emergency that could be avoided with earlier detection.
Cancer and the Consequences of Late Referral
Cancer diagnoses are among the most time-sensitive in medicine. Evidence consistently shows that delays in referral and diagnosis have devastating consequences.
Young people who wait two months or more for a cancer specialist appointment are:
- Twice as likely to experience a lower quality of life
- At double the risk of developing depression
Furthermore, patients who require three or more GP visits before being referred to a specialist face:
- Twice the risk of anxiety
- Increased emotional distress and uncertainty
These delays often result from non-specific symptoms, difficulties accessing appointments, or hesitation to escalate concerns due to system pressures.
The Impact of Delayed Diagnosis on Physical Health
Delayed diagnosis is not merely an inconvenience—it can be life-altering or even fatal. A systematic review examining cancer treatment timelines found that each four-week delay in treatment was associated with an increase in mortality across all common cancer types.
Disease Progression and Reduced Treatment Effectiveness
When diagnosis is delayed:
- Diseases may progress to more advanced stages
- Treatment options may become more aggressive and invasive
- Survival rates can significantly decrease
- Long-term complications are more likely
For chronic illnesses, delays often result in irreversible damage that could have been prevented with timely intervention.
The Mental Health Consequences of Diagnostic Delays
The psychological toll of delayed diagnosis is profound and often underestimated. Living with unexplained symptoms, uncertainty, and worsening health can significantly affect mental wellbeing.
Anxiety, Depression, and Emotional Distress
Prolonged waiting periods commonly lead to:
- Heightened anxiety
- Depressive symptoms
- Loss of trust in the healthcare system
- Feelings of helplessness and frustration
Patients often describe the waiting period as emotionally exhausting, particularly when symptoms interfere with daily life and work.
PTSD-like Distress in Vulnerable Patients
For some individuals, particularly those with pre-existing mental health conditions, delayed diagnosis can result in PTSD-like distress. Repeated appointments, unresolved symptoms, and fear of serious illness create a cycle of stress that can persist long after diagnosis is eventually made.
Navigating the Healthcare System When Something Feels “Off”
Patients are not powerless, even within an overstretched system. Being proactive and informed can make a meaningful difference.
Advocating for Yourself as a Patient
If something doesn’t feel right, trust your instincts. Before requesting a second opinion, it is important to:
- Ask your clinical team to clearly explain the diagnosis
- Request clarification on test results and reasoning
- Ensure all symptoms have been documented
Clear communication can sometimes resolve misunderstandings or prompt further investigation.
Requesting a Second Opinion Through Your GP
If concerns persist, returning to your GP is a crucial step. You can request a new referral specifically marked “for a second opinion.” Your GP will:
- Forward all relevant test results
- Include previous clinical notes
- Ensure continuity of information
While a second opinion consultant will not automatically take over your care, their assessment may differ and open the door to alternative treatment options or earlier intervention.
Transferring Care When Advice Differs
If the second opinion reveals a different diagnosis or treatment approach, you can discuss transferring your care. This decision should be made collaboratively, ensuring that you fully understand the risks, benefits, and next steps.
When Delayed Diagnosis Becomes Medical Negligence
Not all delays constitute negligence. However, when delays fall below an acceptable standard of care and result in avoidable harm, legal recourse may be available.
Understanding Professional Negligence
Medical negligence occurs when a healthcare professional:
- Fails to meet accepted standards of care
- Causes harm through delayed diagnosis or treatment
- Misses opportunities for earlier intervention
Each case is assessed individually, taking into account what a reasonably competent professional would have done under similar circumstances.
Legal Support After a Delayed Diagnosis
Patients who believe they have been harmed by a delayed diagnosis may consider seeking legal advice. The process is governed by specific legal frameworks designed to ensure fairness and accountability.
The Pre-Action Protocol for Professional Negligence
Under the Pre-Action Protocol for Professional Negligence, the claimant should begin by issuing:
- A Preliminary Notice
- A Letter of Claim
These documents give the professional or organisation the opportunity to investigate and respond, usually within three months.
Time Limits Under the Limitation Act 1980
The Limitation Act 1980 generally bars medical negligence claims brought more than three years after:
- The date of injury, or
- The date when the claimant became aware of the harm
There is also a 15-year longstop, after which claims are usually no longer permitted. Understanding these time limits is essential when considering legal action.

The Role of Medical Negligence Solicitors
Medical negligence solicitors play a vital role in helping patients navigate complex legal processes. From Liverpool to London and everywhere in-between, experienced professionals can:
- Assess the merits of a claim
- Gather medical evidence
- Liaise with independent experts
- Support patients throughout the legal journey
Legal action is not about assigning blame unnecessarily, but about accountability, learning, and preventing future harm.
Final Thoughts: Protecting Your Health in a Stretched System
Even trusted healthcare systems can falter under pressure. Delayed diagnosis remains one of the most significant challenges facing modern healthcare in the UK. By understanding which conditions suffer most, recognising the physical and mental impact of delays, and knowing how to advocate for yourself, patients can take proactive steps to protect their health.
Early action matters. Whether it involves seeking a second opinion, pushing for clarity, or obtaining legal advice when harm has occurred, informed patients are better positioned to achieve better outcomes—even in the face of systemic challenges
For more
For more exclusive influencer stories, visit influencergonewild






